1
Distal Radial Physeal Injuries
Gymnast Wrist

Epidemiology: Gymnasts with open growth plates (meaning they are still growing and have not yet finished going through puberty) are at risk for Gymnast wrist.
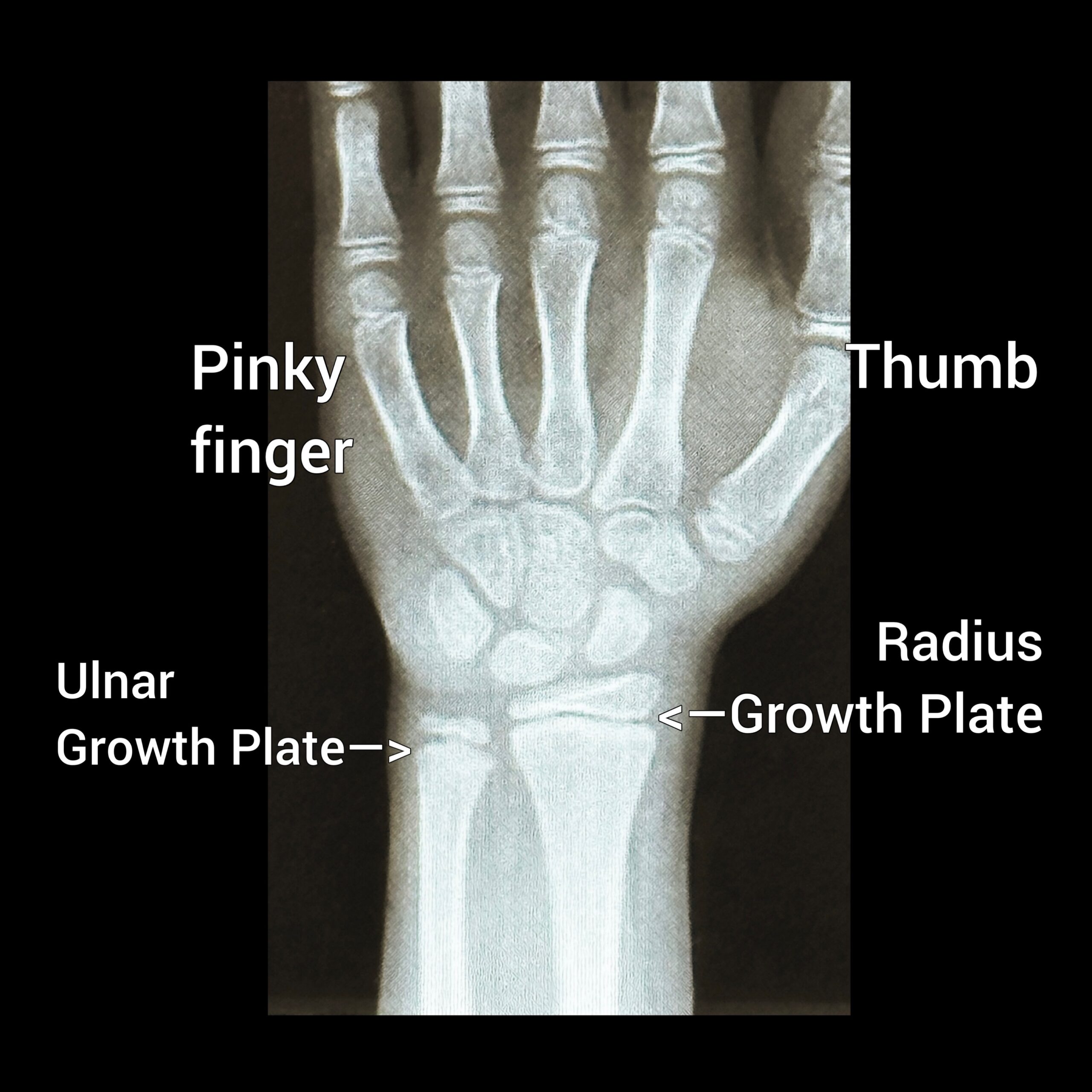
Mechanism of Injury/Description: Gymnast Wrist occurs from repetitive weight-bearing/pounding on the hands (ex: back handspring, vaulting, etc…) which leads to injury/inflammation to the radial growth plate (thumb side) of the wrist.
Signs/Symptoms: On exam, gymnasts may have tenderness to palpation (touch) on the wrist at the growth plates, decreased wrist motion (specifically with wrist extension), and pain with weight bearing on the hands (a positive L hold or seated lift-off test).
Diagnosis: Gymnast Wrist is diagnosed by physical exam (ex: pain with palpation, decreased wrist extension, positive L hold test), x-rays (ex: distal radial physeal widening or early closure, parrot beaked appearance, and sometimes positive ulnar variance), and sometimes an MRI is used in the diagnosis of Gymnast wrist.
Treatment: Rest from impact/pounding, immobilization in a brace or cast, and physical therapy are important in treating Gymnast Wrist. Severe cases may require surgery.
Prevention: To prevent Gymnast Wrist decrease repetitive impact/pounding, strengthen your wrist, shoulder, and periscapular muscles, and use proper technique when performing upper extremity weight bearing gymnastics skills.
Gymnastics Medical Provider PEARLS: When considering Gymnast Wrist as a diagnosis, consider doing bilateral AP x-ray films of the wrist with the elbow at 90 degrees and shoulder abducted to 90 degrees to compare and assess the stage of Gymnast Wrist. There are “3 stages” of gymnast wrist. Grade 1 pain with weight bearing but no radiographic changes, Grade IIa widening at the distal radial physis, Grade IIb early closure of the distal radial physis, and Grade III complete closure of the radial physis and ulnar positive variance.
Gymnast, Parent, and Coach PEARLS: Do NOT ignore wrist pain. If your gymnast is having wrist pain do not put wrist guards on to decrease the pain; instead see a medical provider for a diagnosis/cause of the pain.
1
Distal Radial Physeal Injuries
Gymnast Wrist

Epidemiology: Gymnasts with open growth plates (meaning they are still growing and have not yet finished going through puberty) are at risk for Gymnast wrist.
Mechanism of Injury/Description: Gymnast Wrist occurs from repetitive weight-bearing/pounding on the hands (ex: back handspring, vaulting, etc…) which leads to injury/inflammation to the radial growth plate (thumb side) of the wrist.
Signs/Symptoms: On exam, gymnasts may have tenderness to palpation (touch) on the wrist at the growth plates, decreased wrist motion (specifically with wrist extension), and pain with weight bearing on the hands (a positive L hold or seated lift-off test).
Diagnosis: Gymnast Wrist is diagnosed by physical exam (ex: pain with palpation, decreased wrist extension, positive L hold test), x-rays (ex: distal radial physeal widening or early closure, parrot beaked appearance, and sometimes positive ulnar variance), and sometimes an MRI is used in the diagnosis of Gymnast wrist.
Treatment: Rest from impact/pounding, immobilization in a brace or cast, and physical therapy are important in treating Gymnast Wrist. Severe cases may require surgery.
Prevention: To prevent Gymnast Wrist decrease repetitive impact/pounding, strengthen your wrist, shoulder, and periscapular muscles, and use proper technique when performing upper extremity weight bearing gymnastics skills.
Gymnastics Medical Provider PEARLS: When considering Gymnast Wrist as a diagnosis, consider doing bilateral AP x-ray films of the wrist with the elbow at 90 degrees and shoulder abducted to 90 degrees to compare and assess the stage of Gymnast Wrist. There are “3 stages” of gymnast wrist. Grade 1 pain with weight bearing but no radiographic changes, Grade IIa widening at the distal radial physis, Grade IIb early closure of the distal radial physis, and Grade III complete closure of the radial physis and ulnar positive variance.
Gymnast, Parent, and Coach PEARLS: Do NOT ignore wrist pain. If your gymnast is having wrist pain do not put wrist guards on to decrease the pain; instead see a medical provider for a diagnosis/cause of the pain.
2
Grip Lock
Epidemiology: Any gymnast who wears grips on uneven bars, high bar, or rings, is at risk for grip lock.
Mechanism of Injury/Description: While performing a circling element (ex: giant, clear hip) on one of the above events, the leather grip can overlap or fold over, causing the hand to stay in place while the forearm continues to rotate. This can cause a fracture of the forearm (named Grip Lock).
Signs/Symptoms: Gymnasts will have immediate pain and a deformity of the forearm if they have Grip Lock.
Diagnosis: Grip lock is diagnosed by the history and physical exam which often includes a deformity and tenderness at the ulna and radius. X-rays will show fractures of the radius or ulna.
Treatment: Gymnasts with Grip Lock should seek immediate medical care at the emergency department. Immobilization in a splint or cast, or surgery, may be needed.
Prevention: Wearing proper fitting grips can prevent Grip Lock.
Gymnastics Medical Provider PEARLS: If you are covering a gymnastics competition be sure you are aware of this injury as well as have an EAP (Emergency Action Plan). Gymnasts are sometimes “flung” from the event and may need a full trauma evaluation or they can also be stuck “dangling” from the event. Be prepared in each scenario to safely transport the gymnast to a local Emergency Department/EMS.
Gymnast, Parent, and Coach PEARLS: When purchasing grips always check with the supplier and coaches to be sure your grips are fitting properly. Consider purchasing 2-3 pairs of grips at a time and rotate through the pairs during season.
3
TFCC
Triangular Fibrocartilage Complex Tear
Epidemiology: TFCC tears can occur at any age, but are more likely to happen if the gymnast has a history of Gymnast Wrist with positive ulnar variance (see Gymnast Wrist section above).
Mechanism of Injury/Description: TFCC injuries may occur from a fall or landing with the arm out in front or from repetitive overuse in gymnasts with positive ulnar variance (meaning the ulna bone has grown longer than the radius bone). In positive ulnar variance, the ulna and carpal bones knock into each other causing a degenerative tear.
Signs/Symptoms: Gymnasts will report pain in the wrist on the pinky side (area of TFCC) usually with wrist extension and weight bearing.
Diagnosis: TFCC tears may be suspected based on physical exam findings (see above) and including positive “fovea” sign (find the styloid of the ulna and the flexor carpi ulnaris tendon and between these two landmarks there will be a soft spot and press firmly here; a positive test is pain) or pain with a seated L-hold test.
Treatment: Depending on the severity of your TFCC tear, you can try non-operative (cast/immobilization, NSAIDs, and an injection) or operative (surgical treatment) treatment.
Prevention: Proper hand/weight bearing techniques (wrists turned slightly in), avoiding elbow hyperextension, periscapular strengthening, and having proper posture can help prevent TFCC injuries.
Gymnastics Medical Provider PEARLS: TFCC tears typically occur in gymnasts who have positive ulnar variance which most likely has occurred from gymnast wrist.
Gymnast, Parent, and Coach PEARLS: Do NOT ignore wrist pain. If your gymnast is having wrist pain do not put wrist guards on to decrease the pain; instead see a medical provider for a diagnosis/cause of the pain.
4
Scaphoid Fracture
Epidemiology: The scaphoid is the most frequently fractured carpal (hand) bone and can occur at any age.
Mechanism of Injury/Description: Falling or landing with arm out in front (FOOSH, fall on an outstretched hand) can cause a scaphoid fracture.
Signs/Symptoms: Gymnasts will have pain on the scaphoid bone (which is near the base of the thumb), and explain that he/she had a “FOOSH”.
Diagnosis: A Scaphoid fracture is diagnosed by physical exam (pain to palpation-pushing on the scaphoid bone and pain with moving your thumb). An x-ray usually shows the scaphoid fracture, however, a CT scan or MRI may be needed to confirm the diagnosis.
Treatment: Depending on the type of scaphoid fracture, the gymnast may need a splint, cast, or surgery. A thumb Spica cast or splint is often needed for 6 weeks.
Prevention: Teaching gymnasts to land safely can help prevent scaphoid fractures.
Gymnastics Medical Provider PEARLS: The scaphoid bone has poor blood supply, so if it is unclear if it is fractured or not, the gymnast should still be treated to allow it to heal and consider performing an MRI or CT scan. If not treated properly, it may not heal and surgical fixation might be needed.
Gymnast, Parent, and Coach PEARLS: Do NOT ignore thumb pain. If your gymnast is having thumb pain from a fall, see a medical provider for a diagnosis/cause of the pain.
5
Ganglion Cysts
Epidemiology: Ganglion cysts may occur at any age, but usually are related to a muscle, tendon, ligament, or even wrist bone injury.
Mechanism of Injury/Description: A cyst may occur without an injury but are usually due to a joint or tendon injury. Your medical provider should try to help you figure out the cause of your cyst.
Signs/Symptoms: Gymnasts may report a lump or ball of fluid at the wrist. They are usually not painful unless it pinches or pushes into the joint or on a nerve.
Diagnosis: On a physical exam, the Medical Provider may notice a small lump which is moveable and usually not painful. An ultrasound or MRI can be used to help determine the cause of the cyst.
Treatment: Rest, aspiration (removing the fluid), surgery, and determining the cause of the cyst are important in treating ganglion cysts.
Prevention: Proper hand/weight bearing techniques (wrists turned slightly in), avoiding elbow hyperextension, periscapular strengthening, and using correct posture can help to prevent ganglion cysts.
Gymnastics Medical Provider PEARLS: It is important to determine the cause of the cyst; in gymnasts there is typically another injury “brewing” which has led to the cyst formation.
Gymnast, Parent, and Coach PEARLS: Cysts are usually benign and painless but it is important to understand the cause and so seeing a medical provider is advised.

![tfcc tear – shutterstock_2189367401 [Converted]](https://gymnasticsmedicinemens.org/wp-content/uploads/2023/05/tfcc-tear-shutterstock_2189367401-Converted-scaled.jpg)
![scaphoid fracture – shutterstock_1310439049 [Converted]](https://gymnasticsmedicinemens.org/wp-content/uploads/2023/05/scaphoid-fracture-shutterstock_1310439049-Converted.jpg)
