1
Concussion
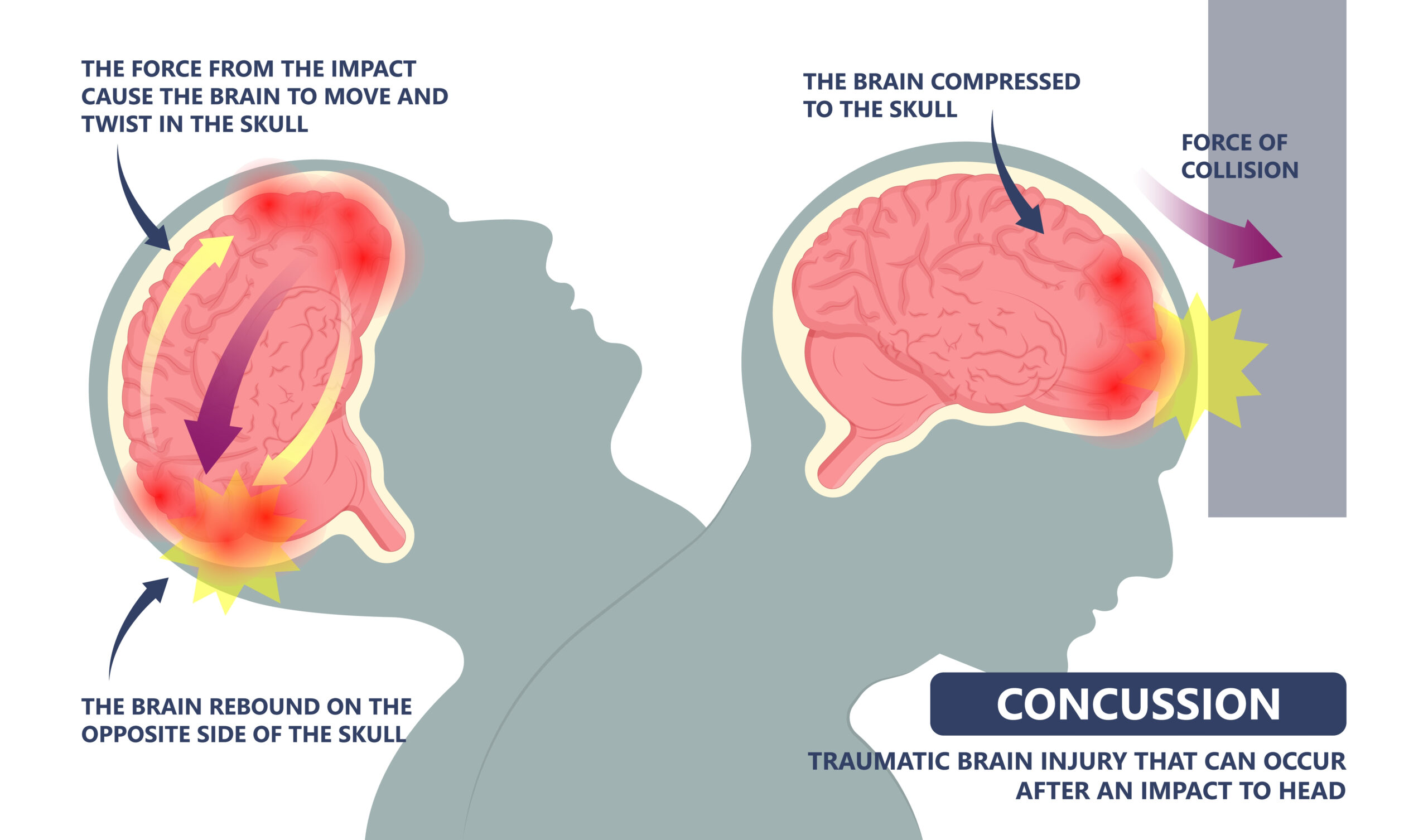
Epidemiology: Can occur at any age.
Mechanism of Injury/Description: A direct blow/hit to the head/neck/face, or any impact force to the head can cause a concussion. This injury is also known as a mild traumatic brain injury (TBI).
Signs/Symptoms: The gymnast will experience headaches, dizziness, nausea/vomiting, balance problems, vision changes, difficulty concentrating, feeling “in a fog”, irritability, and changes to sleep patterns.
Diagnosis: A concussion can be diagnosed by physical exam with testing of Cranial nerves/concussion screen, BESS testing, and/or a sideline evaluation (SCAT 5). A CT scan or MRI may be ordered depending on severity and duration of the gymnast’s signs/symptoms.
Treatment: Immediately remove the gymnast from practice or competition and have the athlete do cognitive and physical rest for 24-48 hours and see a medical provider. Once you have been seen by a medical provider and receive clearance, a gradual progression back into gymnastics should be performed. Please see USAG Concussion Information.
Prevention: To prevent a concussion practice neck strengthening exercises and consider having each gymnast do a baseline IMPACT test prior to the start of each season. Check with local medical providers to see if they are offering this testing.
Gymnastics Medical Provider PEARLS: Gymnastics requires a significant amount of proprioception and balance and with a concussion this can sometimes take gymnasts longer to progress back in. Review over the guidelines and information put together by USA Gymnastics (link above) and see our blog on Concussion education.
Gymnast, Parent, and Coach PEARLS: If a concussion is suspected, stop the practice/competition and have your gymnast see a medical provider for evaluation.
Complications of concussion:
- Second Impact Syndrome
- Post concussion Syndrome
- Intracranial hemorrhage
- CTE (chronic traumatic Encephalopathy)
For more information, read our blog on Concussion Education.
1
Concussion
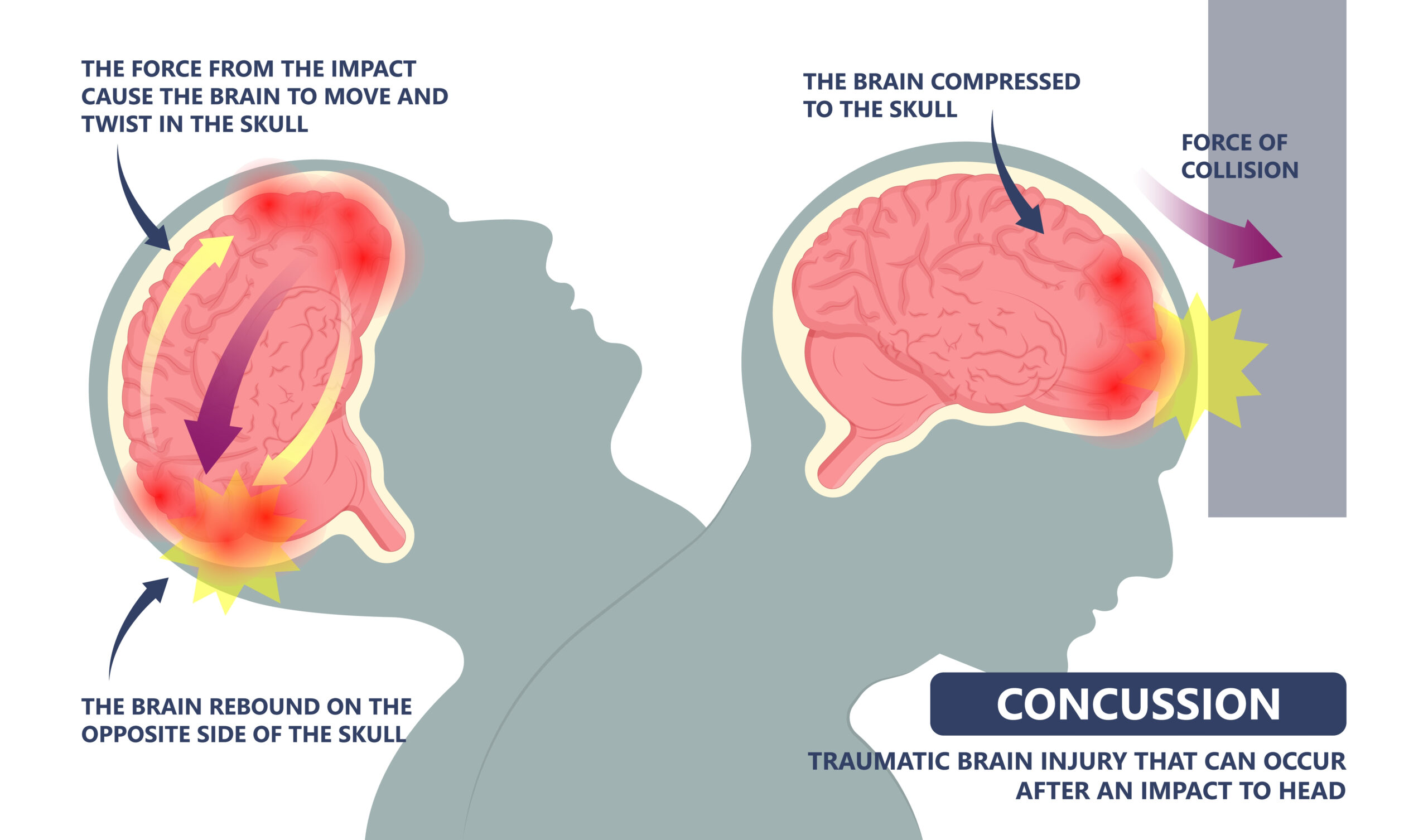
Epidemiology: Can occur at any age.
Mechanism of Injury/Description: A direct blow/hit to the head/neck/face, or any impact force to the head can cause a concussion. This injury is also known as a mild traumatic brain injury (TBI).
Signs/Symptoms: The gymnast will experience headaches, dizziness, nausea/vomiting, balance problems, vision changes, difficulty concentrating, feeling “in a fog”, irritability, and changes to sleep patterns.
Diagnosis: A concussion can be diagnosed by physical exam with testing of Cranial nerves/concussion screen, BESS testing, and/or a sideline evaluation (SCAT 5). A CT scan or MRI may be ordered depending on severity and duration of the gymnast’s signs/symptoms.
Treatment: Immediately remove the gymnast from practice or competition and have the athlete do cognitive and physical rest for 24-48 hours and see a medical provider. Once you have been seen by a medical provider and receive clearance, a gradual progression back into gymnastics should be performed. Please see USAG Concussion Information.
Prevention: To prevent a concussion practice neck strengthening exercises and consider having each gymnast do a baseline IMPACT test prior to the start of each season. Check with local medical providers to see if they are offering this testing.
Gymnastics Medical Provider PEARLS: Gymnastics requires a significant amount of proprioception and balance and with a concussion this can sometimes take gymnasts longer to progress back in. Review over the guidelines and information put together by USA Gymnastics (link above) and see our blog on Concussion education.
Gymnast, Parent, and Coach PEARLS: If a concussion is suspected, stop the practice/competition and have your gymnast see a medical provider for evaluation.
Complications of concussion:
- Second Impact Syndrome
- Post concussion Syndrome
- Intracranial hemorrhage
- CTE (chronic traumatic Encephalopathy)
For more information, read our blog on Concussion Education.
2
Orbital Wall Fracture
Epidemiology: Can occur at any age.
Mechanism of Injury/Description: An orbital wall fracture occurs from a direct blow or hit to the eye/orbital region causing a fracture and then the inability to move your eye.
Signs/Symptoms: The gymnast will experience pain, blurry or double vision, swelling/inflammation, and an inability to move the eye.
Diagnosis: The diagnosis is determined by physical exam (pain, blurry or double vision, swelling/inflammation, and an inability to move the eye), and an immediate referral to an ophthalmologist.
Treatment: Treatment is an immediate referral to an ophthalmologist.
Prevention: Prevention of an orbital wall fracture is to avoid getting hit in the eye.
Gymnastics Medical Provider PEARLS: This usually occurs with an acute fall/hit so make sure you do a full trauma exam/workup to rule out other serious injuries.
Gymnast, Parent, and Coach PEARLS: This is a medical emergency. If this is seen in a gymnast after a trauma/hit to the eye immediately have the gymnast go to the emergency department.
3
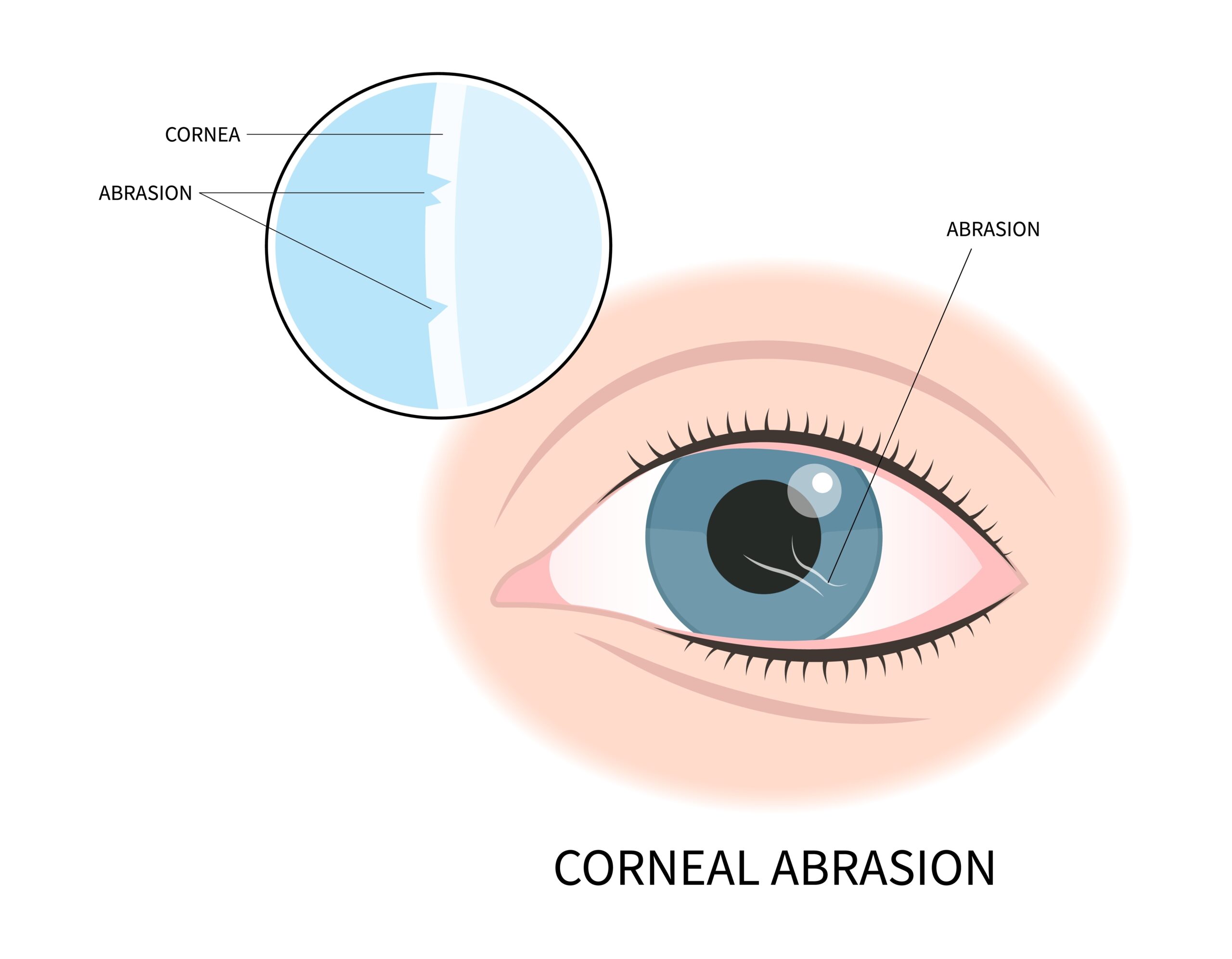
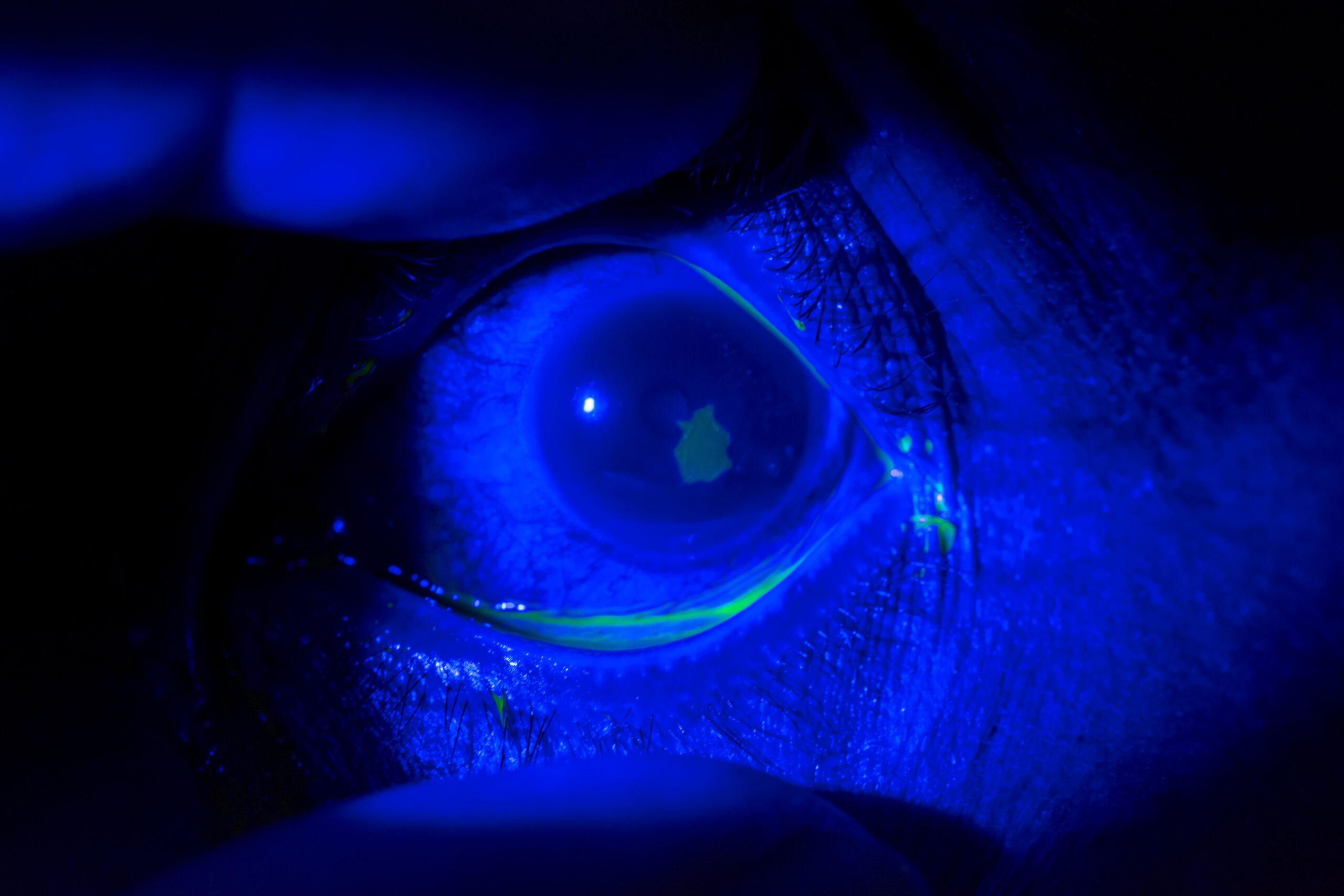
Corneal Abrasion
Epidemiology: Can occur at any age.
Mechanism of Injury/Description: A corneal abrasion occurs by having an injury to the eye’s cornea which can be from chalk or another particle that enters the eye and scratches/damages the cornea.
Signs/Symptoms: The gymnast will experience pain in the eye, redness, and blurred vision.
Diagnosis: A corneal abrasion is diagnosed by physical exam and fluorescent stain with UV light.
Treatment: Treatment for a corneal abrasion includes topical NSAIDs, antibiotics, eye patch, and a non-urgent referral to ophthalmologist.
Prevention: To prevent this injury avoid foreign objects in eyes.
Gymnastics Medical Provider PEARLS: Have a fluorescent stain with UV light available in your medical kit when covering a gymnastics competition. Also consider having saline to flush the eye out.
Gymnast, Parent, and Coach PEARLS: If you suspect something has gone into your eye, stop what you are doing, tell an adult, wash your hands, and then go to an area where you can flush your eye out with water gently. If this does not work or you have worsening pain or redness see a medical provider.
4
Hyphema
Epidemiology: Can occur at any age.
Mechanism of Injury/Description: A hyphema is when blood goes into the anterior chamber of the eye from a direct blow/hit to the eye.
Signs/Symptoms: The gymnast will experience eye pain, blurred vision, and red fluid accumulating in the eye.
Diagnosis: This is diagnosed by physical exam and medical emergency/transport to an ophthalmologist.
Treatment: Eye patch and immediate medical emergency/transport to an ophthalmologist.
Prevention: Prevention of a hyphema is to avoid getting hit in the eye.
Gymnastics Medical Provider PEARLS: This usually occurs with an acute fall so make sure you do a full trauma exam/workup to rule out other serious injuries. Also, treatment usually begins by elevating the head of the bed to 30 degrees.
Gymnast, Parent, and Coach PEARLS: This is a medical emergency. If this is seen in a gymnast after a trauma/hit to the eye immediately have the gymnast go to the emergency department.
![ORBIT – shutterstock_1779299549 [Converted]](https://gymnasticsmedicinemens.org/wp-content/uploads/2023/05/ORBIT-shutterstock_1779299549-Converted.jpg)
![hyphema – shutterstock_2155057675 [Converted]](https://gymnasticsmedicinemens.org/wp-content/uploads/2023/05/hyphema-shutterstock_2155057675-Converted.jpg)