1
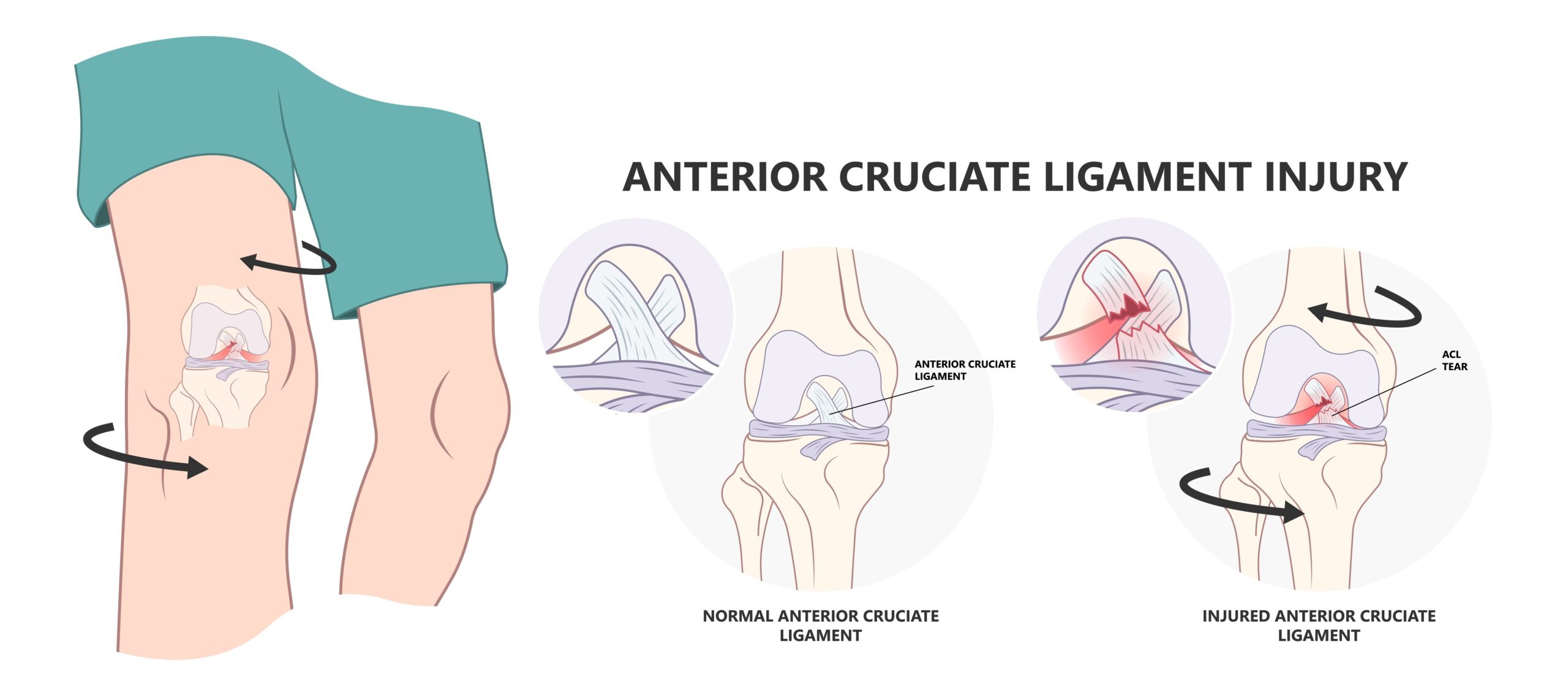
Anterior Cruciate Ligament (ACL) Tear
Epidemiology: An ACL tear can occur at any age and is more common in females.
Mechanism of Injury/Description: An ACL tear occurs with a “plant and twisting” injury, meaning when the gymnast performs a twisting salto/flip and their foot plants/lands, but their body keeps spinning this causes the tear. The ACL stops the knee from shifting forward meaning it prevents anterior translation of the tibia relative to the femur.
Signs/Symptoms: The gymnast will experience pain, swelling (inflammation) of the knee, and feelings of instability or looseness if he/she has an ACL tear.
Diagnosis: An ACL tear is diagnosed by physical exam with a positive anterior drawer, Lachmen, and pivot shift test (all special tests performed by a medical provider in Orthopedics/Sports Medicine). An x-ray is usually ordered to evaluate the bone but an MRI is the definitive test and will show an ACL tear.
Treatment: The treatment for an ACL tear is surgery and usually there is a six to twelve month recovery time prior to returning to full gymnastics.
Prevention: To prevent an ACL injury focus on gluteus, hip, and hamstring strength, and practicing proper landing mechanics (avoid valgus/knocked knees landing).
Gymnastics Medical Provider PEARLS: There are all different types of ACL grafts to choose from. A completely skeletally immature athlete should consider an ITB physeal spearing ACL, a preteen/skeletally immature athlete should consider ITB physeal spearing ACL, hamstring graft autograft, and pending puberty status patellar tendon autograft, an athlete who is skeletally mature should consider a patellar tendon autograft or hamstring authograft, and an older patient who is not as athletic could consider a cadaver graft.
Gymnast, Parent, and Coach PEARLS: An ACL which is torn does need to be reconstructed and so if this is suspected, meet with a pediatric sports medicine surgeon or adolescent sports medicine surgeon (pending your gymnasts’ age).
2
Tibial Tubercle Apophysitis
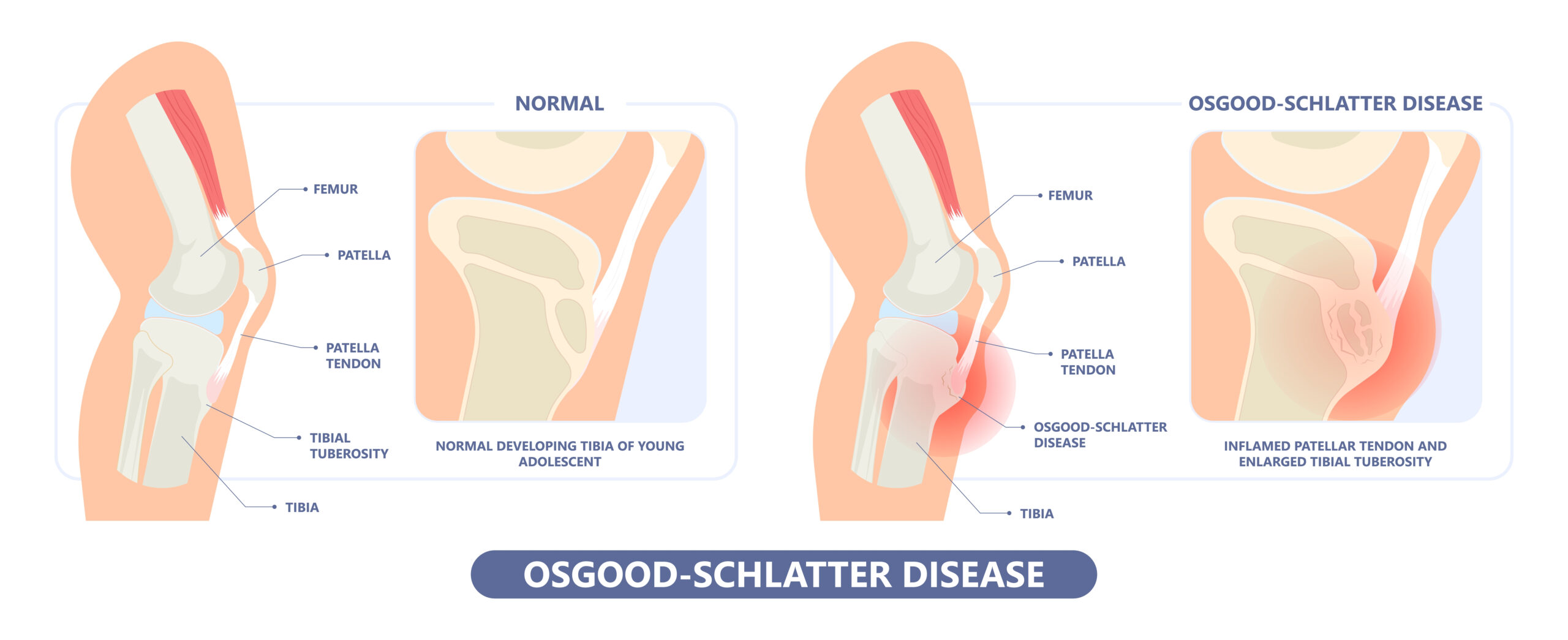
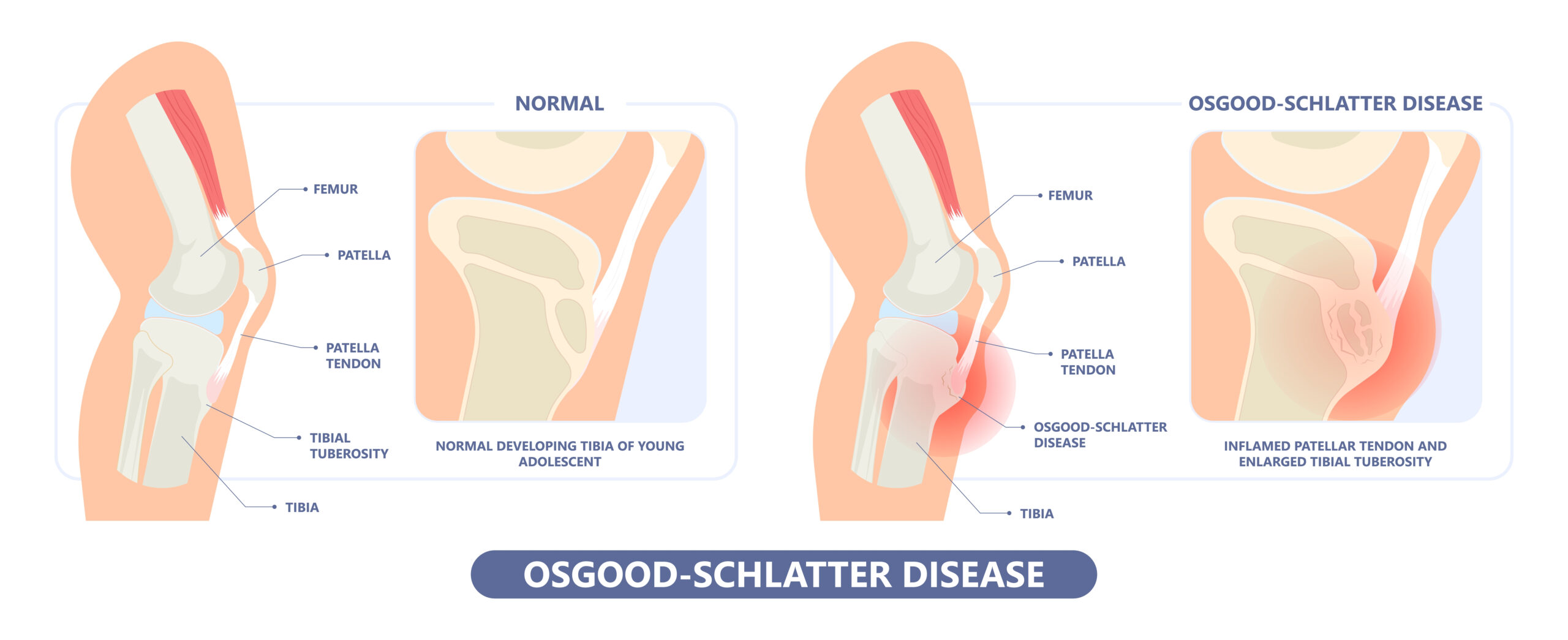
Osgood Schlatter’s Disease
Epidemiology: Osgood Schlatter’s Disease occurs in gymnasts with open growth plates, meaning they are still growing and have not yet finished going through puberty.
Mechanism of Injury/Description: Osgood Schlatter’s Disease is an injury to the tibial tubercle growth plate from the patellar tendon “tugging”/contracting and pulling on the tibial tubercle (where there is a growth plate) causing inflammation and pain (also called traction apophysitis).
Signs/Symptoms: The gymnast will have anterior (front) knee pain with tenderness to touch on the shin bone (tibial tubercle) and pain when he/she tries to extend (straighten) their knee against resistance. The gymnast may also have pain with running, jumping, and landing.
Diagnosis: The diagnosis for Osgood Schlatter’s Disease is determined by physical exam with tenderness to palpate/push on the tibial tubercle, pain with resisted knee extension, enlarged/prominent tibial tubercle, and tight/inflexible quadriceps muscles/a positive Ely test. A lateral x-ray may show widening at the tibial tubercle and this is important to view as there is a risk of a potential avulsion fracture if not treated.
Treatment: Treatment for Osgood Schlatter’s Disease includes rest from pounding/impacting/ landing, physical therapy (with a focus on quad/hip flexor flexibility, gluteus/hip strengthening, and proper landing mechanics), and then a gradual progression back to gymnastics.
Prevention: To prevent this injury focus on quadriceps flexibility and splits with square hips, decreasing repetitive impact/pounding on growing bodies, and practicing proper landing mechanics.
Gymnastics Medical Provider PEARLS: The growth plate typically does not fuse with the tibia until age 14-18 years old. Continue to monitor s/s of Osgood Schlatter’s Disease as some athletes tend to push through the pain and can cause avulsion fractures.
Gymnast, Parent, and Coach PEARLS: Gymnasts can try chopat© straps with either pre-wrap of the traditional strap to take “tension” off the tendon. Coaches, focus on your gymnasts having square hips when performing splits.
2
Tibial Tubercle Apophysitis
Osgood Schlatter’s Disease
Epidemiology: Osgood Schlatter’s Disease occurs in gymnasts with open growth plates, meaning they are still growing and have not yet finished going through puberty.
Mechanism of Injury/Description: Osgood Schlatter’s Disease is an injury to the tibial tubercle growth plate from the patellar tendon “tugging”/contracting and pulling on the tibial tubercle (where there is a growth plate) causing inflammation and pain (also called traction apophysitis).
Signs/Symptoms: The gymnast will have anterior (front) knee pain with tenderness to touch on the shin bone (tibial tubercle) and pain when he/she tries to extend (straighten) their knee against resistance. The gymnast may also have pain with running, jumping, and landing.
Diagnosis: The diagnosis for Osgood Schlatter’s Disease is determined by physical exam with tenderness to palpate/push on the tibial tubercle, pain with resisted knee extension, enlarged/prominent tibial tubercle, and tight/inflexible quadriceps muscles/a positive Ely test. A lateral x-ray may show widening at the tibial tubercle and this is important to view as there is a risk of a potential avulsion fracture if not treated.
Treatment: Treatment for Osgood Schlatter’s Disease includes rest from pounding/impacting/ landing, physical therapy (with a focus on quad/hip flexor flexibility, gluteus/hip strengthening, and proper landing mechanics), and then a gradual progression back to gymnastics.
Prevention: To prevent this injury focus on quadriceps flexibility and splits with square hips, decreasing repetitive impact/pounding on growing bodies, and practicing proper landing mechanics.
Gymnastics Medical Provider PEARLS: The growth plate typically does not fuse with the tibia until age 14-18 years old. Continue to monitor s/s of Osgood Schlatter’s Disease as some athletes tend to push through the pain and can cause avulsion fractures.
Gymnast, Parent, and Coach PEARLS: Gymnasts can try chopat© straps with either pre-wrap of the traditional strap to take “tension” off the tendon. Coaches, focus on your gymnasts having square hips when performing splits.
3
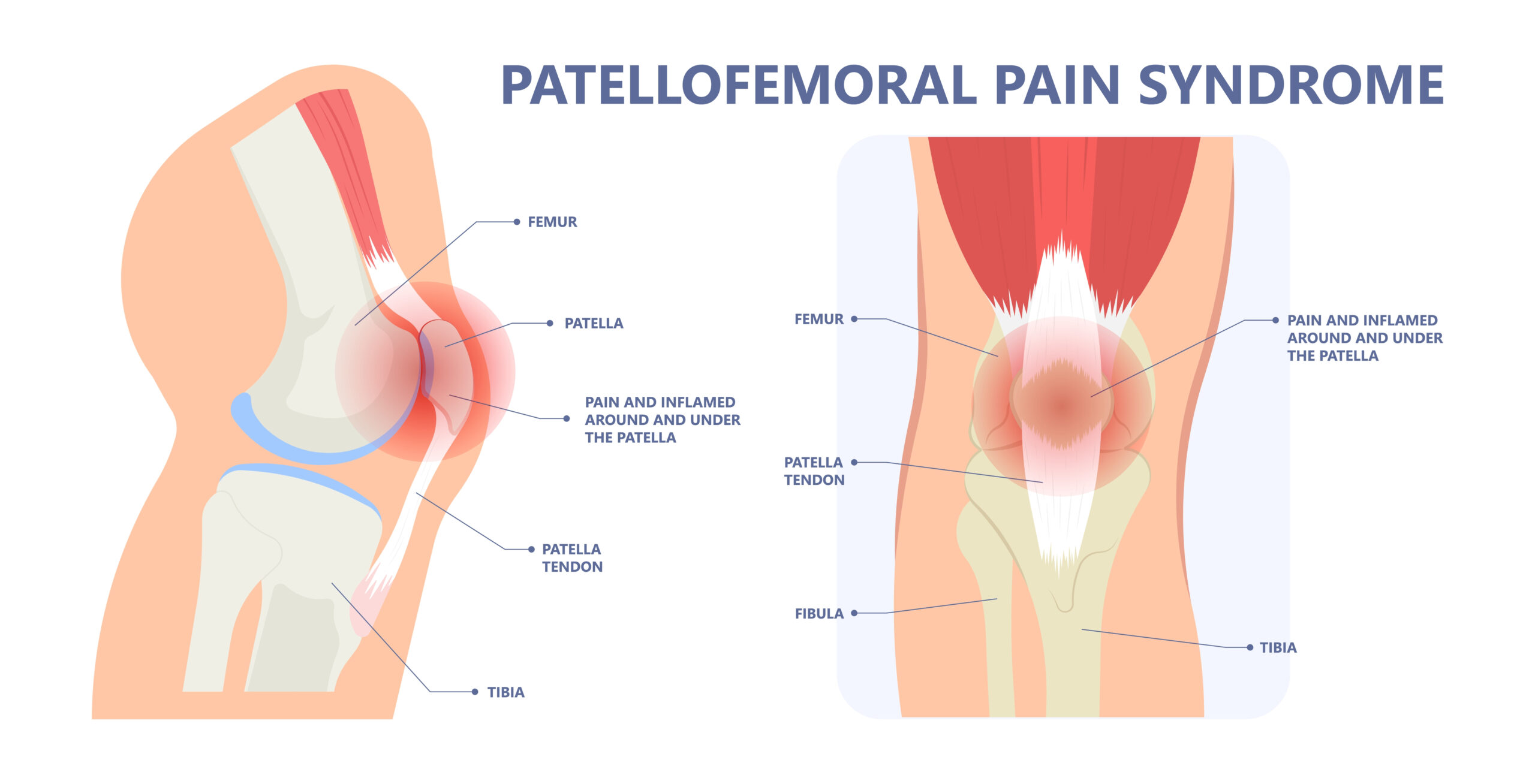
Patellofemoral Syndrome
Epidemiology: Patellofemoral Syndrome occurs mainly in females due to puberty and “developing hips”, which causes an increased “Q angle”.
Mechanism of Injury/Description: Patellofemoral Syndrome results from abnormal patellofemoral tracking causing inflammation, pain, and possible cartilage injury. When gymnasts go through puberty and experience growth in the hip region, this causes an increased Q angle which changes the way the patella sits in the patellofemoral joint and additionally with muscles imbalances this causes the patella to not track properly leading to inflammation, pain, and possible cartilage injury.
Signs/Symptoms: Signs and symptoms of patellofemoral syndrome include but are not limited to chronic knee pain in the shape of a “C”, decreased muscle bulk of the vastus medialis (VMO), pain with jumping/pounding/landing, and an increased Q angle.
Diagnosis: The diagnosis of patellofemoral syndrome is determined by a physical exam which shows a positive Ober’s test, “C” shaped pain, increased Q angle, and a lateral patellar tilt. An x-ray should also be obtained and on the sunrise view it will most likely show a lateral patellar tilt.
Treatment: Treatment for patellofemoral syndrome includes rest from impact/pounding and physical therapy with a focus on lateral stretching and medial strengthening. RICE (Rest, Ice, Compression, Elevation) and anti-inflammatory medication may also be recommended.
Prevention: Prevention of patellofemoral syndrome should include VMO strength, stretching hip flexors and ITB, practicing proper landing mechanics, and avoiding valgus/knocked knees landing.
Gymnastics Medical Provider PEARLS: Consider ordering an MRI even if you suspect the diagnosis is patellofemoral syndrome as you want to be sure you are not missing any cartilage damage, or ligaments injury that may require more invasive treatment.
Gymnast, Parent, and Coach PEARLS: Look at your gymnasts landing mechanics to be sure he/she is not landing with a valgus collapse (knees knocked in) this can lead to increased knee pain and injuries.
4
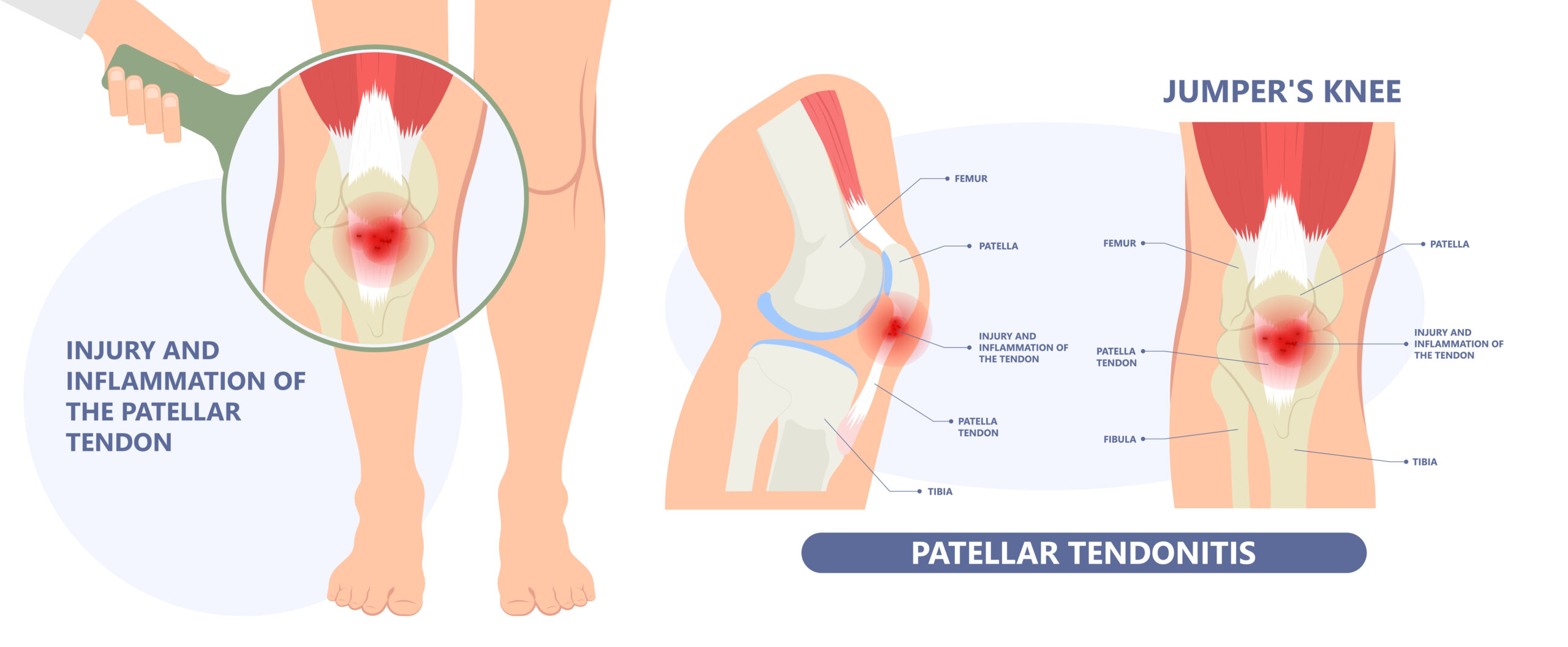
Jumper’s Knee
Patellar Tendonitis
Epidemiology: Patellar tendonitis can occur at any age but is more common in adolescents, males, and “jumping” athletes.
Mechanism of Injury/Description: Inflammation (swelling) to the patellar tendon which occurs from eccentric contraction of the extensor mechanism (repetitive jumping/landing).
Signs/Symptoms: The gymnast will have anterior (front) knee pain with tenderness to touch on the patellar tendon between patella (the knee cap) and the tibial tubercle (shin bone). The gymnast will describe pain during and/or after jumping/landing skills.
Diagnosis: To diagnose patellar tendonitis your Medical Provider will perform a physical exam showing tenderness to palpate/push on the patellar tendon, pain with resisted knee extension, and tight/inflexible quadriceps muscles (a positive Ely test). X-rays are recommended to rule out other causes of anterior (front) knee pain.
Treatment: To treat patellar tendonitis gymnasts should rest from pounding/impacting/landing, do physical therapy (with a decreasing pain/inflammation with modalities, focus on quad/hip flexor flexibility, gluteus/hip strengthening, and work on proper landing mechanics), and then once cleared by your Medical Provider use a gradual progression back to gymnastics. RICE (Rest, Ice, Compression, Elevation) and anti-inflammatory medication may also be recommended.
Prevention: To prevent this injury, focus on quadriceps flexibility and splits with square hips, decreasing repetitive impact/pounding on growing bodies, and practicing proper landing mechanics.
Gymnastics Medical Provider PEARLS: Consider ordering an MRI if the gymnast’s pain does not go away or if the gymnast continues to have reoccurring patellar tendonitis as this could indicate that there may be other causes of pain or perhaps tendon thickening which may require surgical intervention.
Gymnast, Parent, and Coach PEARLS: Do not encourage your gymnast to get a cortisone injection as these are contraindicated and can lead to tendon rupture.
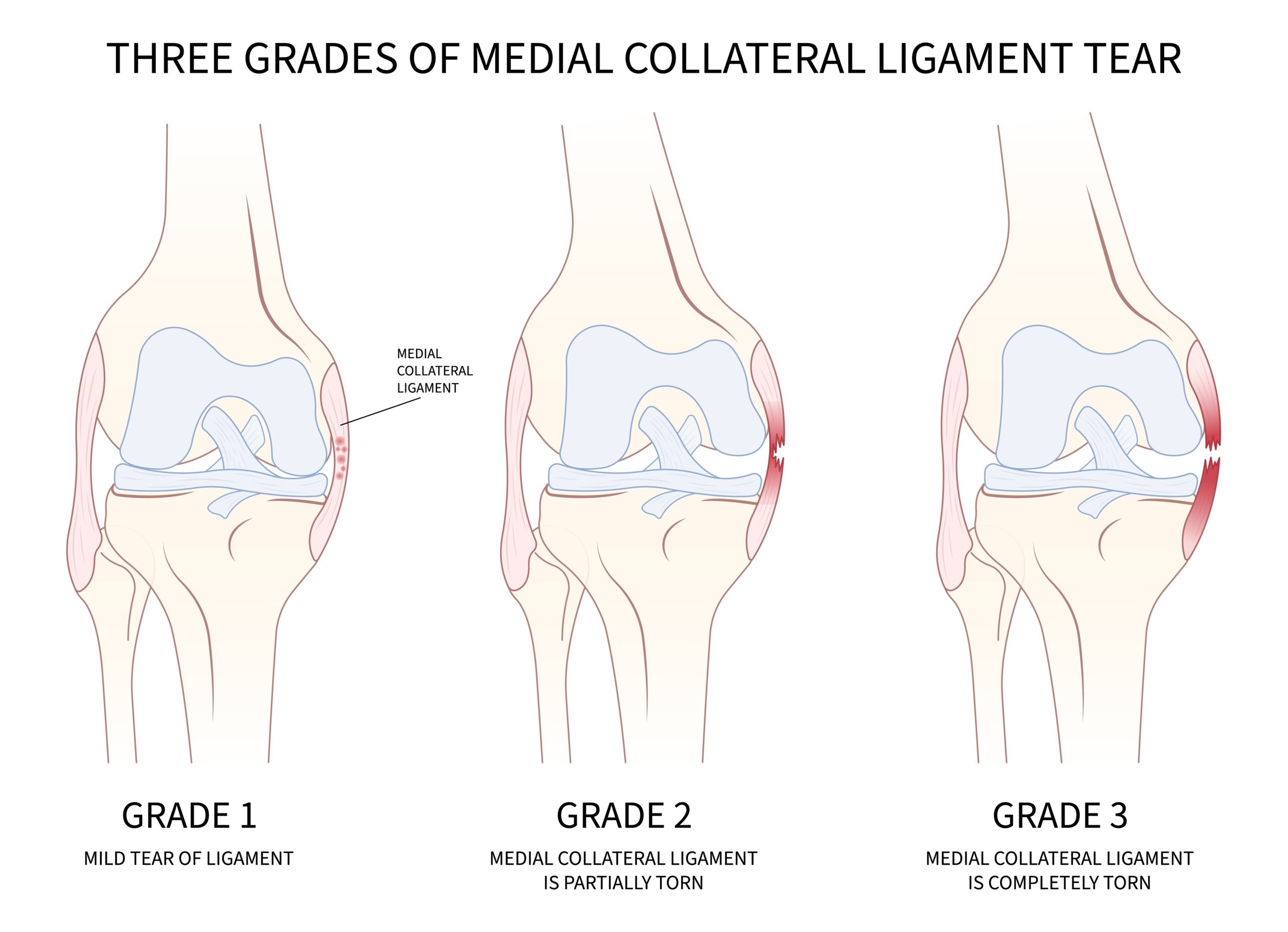
5
Medial Collateral Ligament (MCL) /Lateral Collateral Ligament (LCL) Sprain/Tear
Epidemiology: Can occur at any age. Per Orthobullets© isolated LCL tears are most commonly seen in gymnasts and tennis players.
Mechanism of Injury/Description: An MCL injury refers to when a plant and inward/valgus force occurs, while an LCL injury refers to a plant and outward/varus force occurring.
Signs/Symptoms: There will be medial (inward) pain of the knee for an MCL injury, and lateral (outward) pain for an LCL injury.
Diagnosis: An MCL or LCL injury is diagnosed by physical exam and an MRI. For an MCL tear there will be pain on the medial (inside) aspect of the knee and a positive valgus stress test. For an LCL tear there will be pain on the lateral (outside) aspect of the knee and a positive varus stress test and positive dial test.
Treatment: Treatment usually depends on the grade/severity of the injury. Grades 1-2 usually require rest, brace, physical therapy, but in some cases (and with some Grade 3) it may require surgical intervention.
Prevention: To prevent MCL and LCL injuries focus on gluteus, hip, and hamstring strength, practicing proper landing mechanics (avoid valgus/knocked knees landing).
Gymnastics Medical Provider PEARLS: Per Orthobullets© the MCL is the most common ligament injured in the knee (40%) and proximal tears have greater healing rates than distal tears. An MCL tear is also usually associated with an ACL tear. Pellegrini-Stieda Syndrome can sometimes be seen on x-ray (calcification at the medial femoral insertion site) with an MCL tear. Isolated LCL injuries are very rare. If an LCL injury is suspected, also investigate for a posterior corner injury.
Gymnast, Parent, and Coach PEARLS: If your gymnast has an MCL or LCL tear make sure your Medical Provider rules out any other ligament or cartilage injury as it is rare to have isolated ligament tears.
6
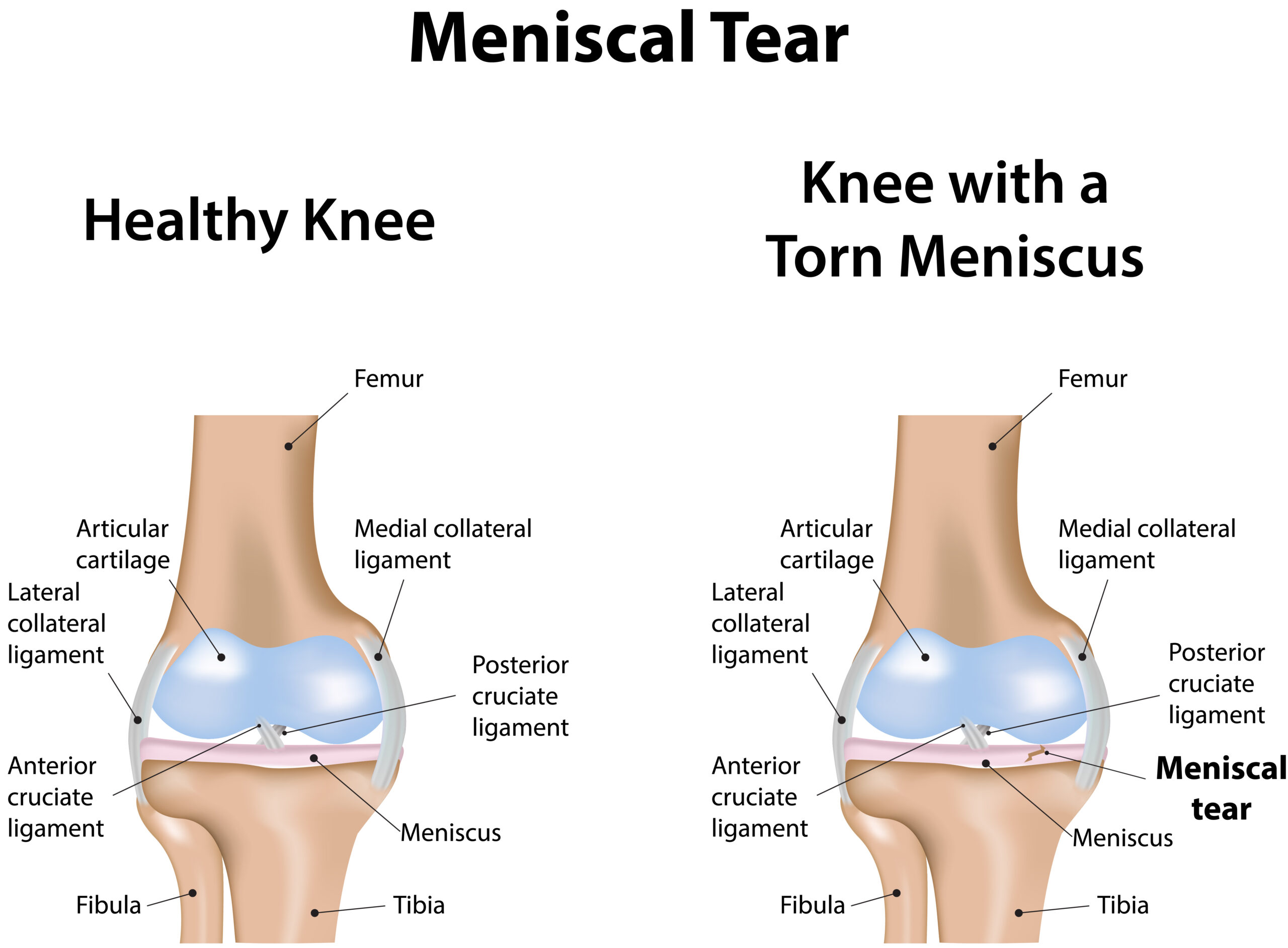
Meniscus Tear
Epidemiology: Can occur at any age and is the most common reason to have knee surgery.
Mechanism of Injury/Description: Typically, a meniscus injury occurs from a twisting mechanism or deep knee flexion. Meniscus is cartilage and is described as the shock absorber of the knee. You have two menisci in your knee: a medial (inside) and lateral (outside).
Signs/Symptoms: The gymnast will experience swelling, pain on the medial or lateral joint line, and clicking/catching/locking (also known as mechanical symptoms).
Diagnosis: The diagnosis is determined by a physical exam when there is pain on the medial or lateral joint line to palpation (touch), and a positive McMurray’s test and Apley compression test. An MRI will also show a meniscus tear.
Treatment: If your gymnast has a meniscus tear, surgery is typically recommended for either a repair or an excision (depending on the location of the tear). Recovery from surgery depends on the type of surgery (repair vs excision).
Prevention: To prevent meniscus tears focus on gluteus, hip, and hamstring strength, and practicing proper landing mechanics (avoid valgus/knocked knees landing).
Gymnastics Medical Provider PEARLS: When considering a repair vs excision of the meniscus during an arthroscopic procedure consider which zone the tear is in: red zone (outer third, vascularized), red-white zone (middle third), and white zone (inner third, avascular).
Gymnast, Parent, and Coach PEARLS: An isolated meniscus repair or excision is typically a day surgical procedure meaning the gymnast has his/her surgery that day and goes home that day. This is the most common surgery for a gymnast to have.
7
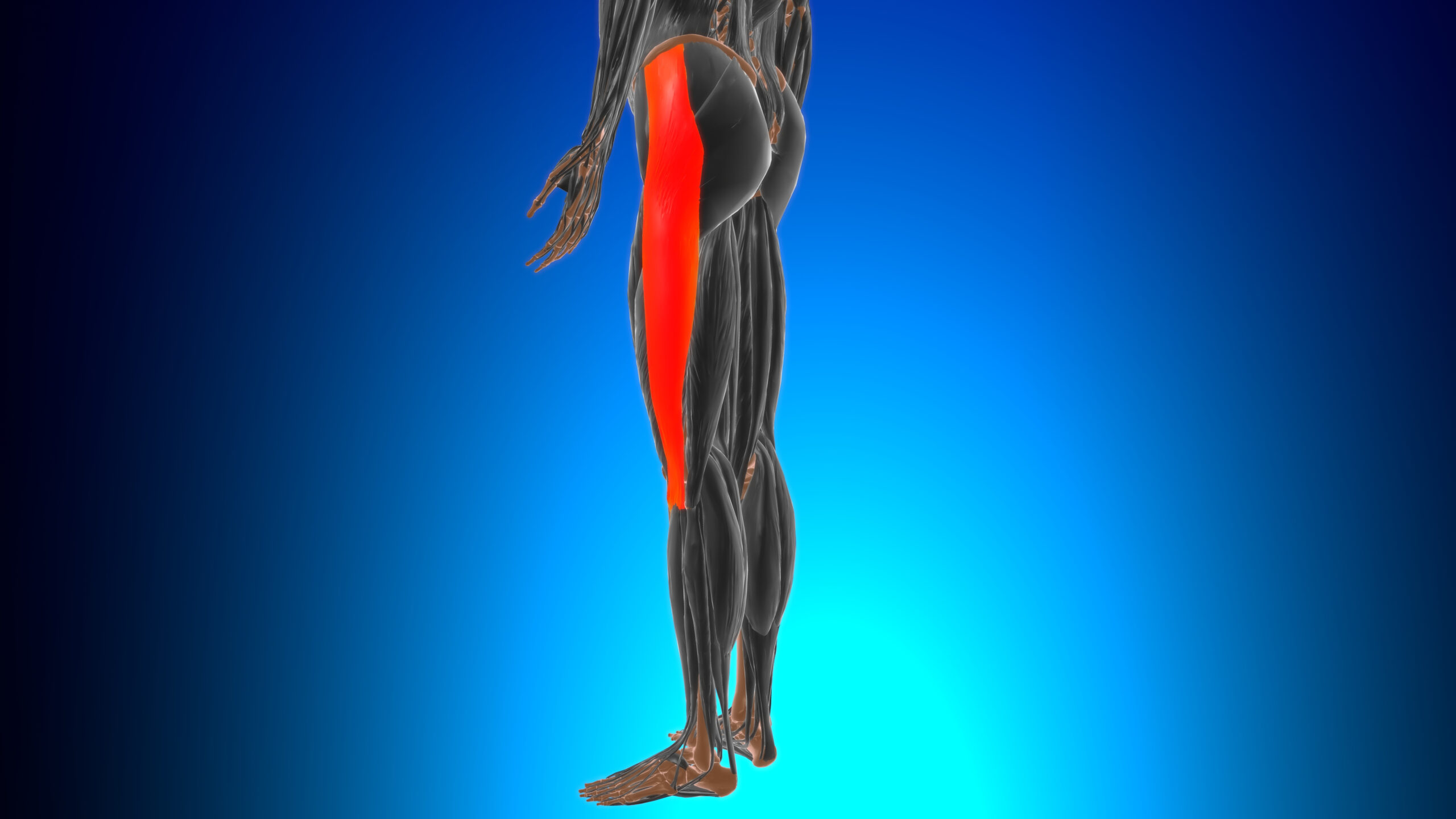
ITB (Iliotibial Band) Friction Syndrome
Epidemiology: ITB friction syndrome can occur at any age and occurs more commonly in athletes who perform repetitive flexion and extension at the knee (ex: runners, cyclists, etc…).
Mechanism of Injury/Description: ITB friction syndrome occurs from repetitive rubbing/friction on the lateral condyle where the ITB attaches which leads to inflammation and pain.
Signs/Symptoms: Signs and symptoms of ITB friction syndrome include but are not limited to pain on the lateral femoral condyle (insertion of the ITB), inflammation, decreased knee motion, pain with jumping/landing, weakness with resisted range of motion testing with hip abduction, and the pain typically goes away with rest.
Diagnosis: ITB friction syndrome is diagnosed by physical exam with pain on the attachment of the ITB (lateral femoral condyle), weakness with resisted range of motion testing with hip abduction, pain with a single leg squat, and a positive Ober test.
Treatment: Treatment for ITB friction syndrome includes but is not limited to rest from impact/pounding, and physical therapy. RICE (Rest, Ice, Compression, Elevation) and anti-inflammatory medication may also be recommended.
Prevention: To prevent this injury focus on VMO strengthening, stretching hip flexors and ITB, and practicing proper landing mechanics (avoid valgus/knocked knees landing).
Gymnastics Medical Provider PEARLS: It is still recommended to order x-rays and even an MRI for this diagnosis if you want to be sure you are ruling out cartilage, bone, and ligamentous injuries. Associated conditions with ITB friction syndrome include medial compartment osteoarthritis, greater trochanteric pain syndrome, and patellofemoral syndrome. Look for these associated conditions when you are evaluating your gymnast.
Gymnast, Parent, and Coach PEARLS: Focus on proper balanced stretching to help prevent this injury. Studies have shown that 50-90% (OrthoBullets©) of patients will improve with 4-8 weeks of non-operative treatment (ex: physical therapy, RICE, etc…) be patient as your gymnast is healing.
8
Patellar Subluxation/Dislocation
Patellar Subluxation/
Dislocation
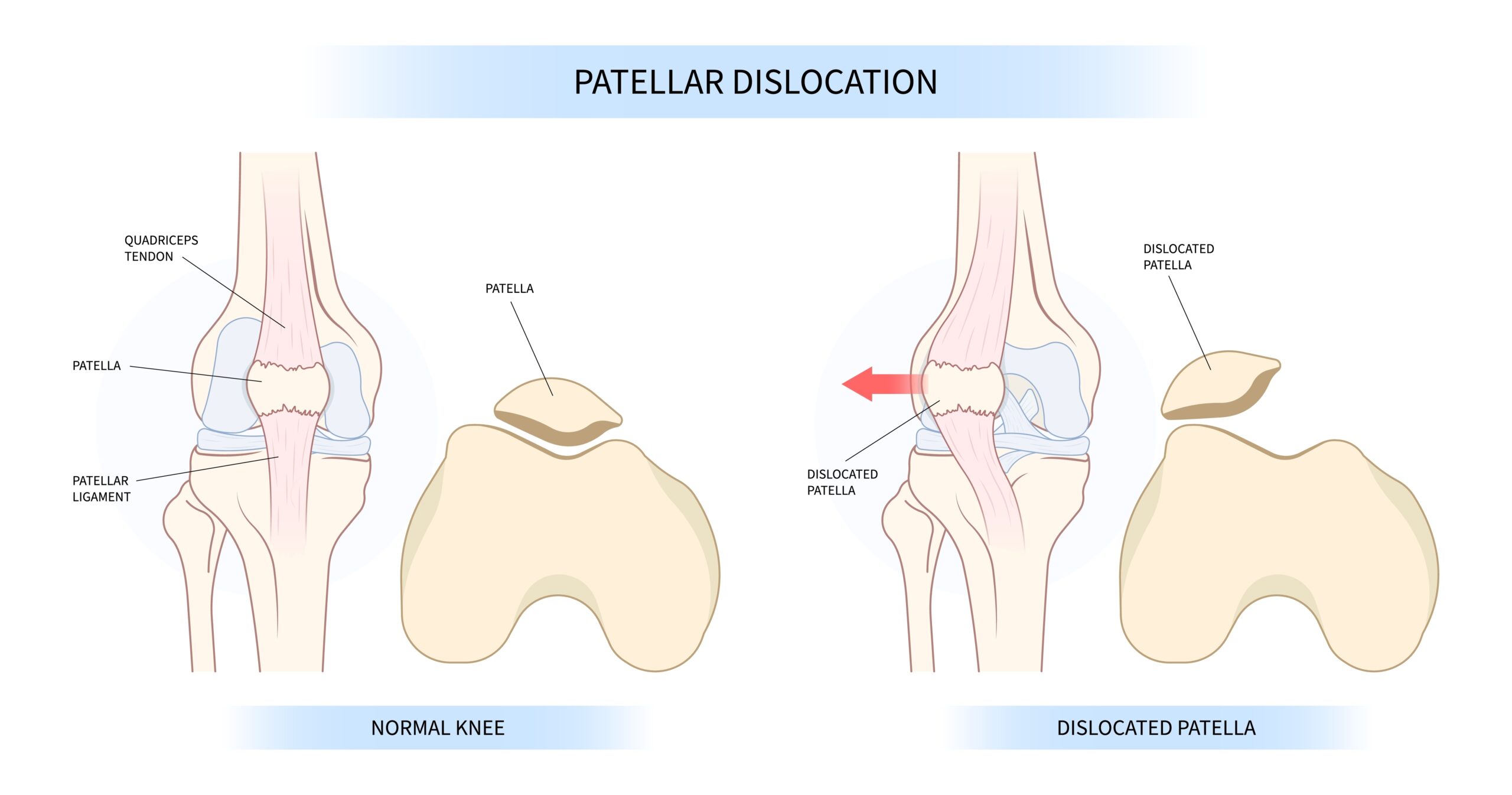
Epidemiology: A patella subluxation of dislocation can occur at any age. Some athletes may have “miserable malalignment syndrome” (external tibial torsion / pronated feet, genu valgum, and femoral anteversion) which predisposes them to having a subluxation or dislocation episode. Athletes who have patella alta (high riding patella), decreased VMO muscle bulk, and tight lateral structures are also predisposed to have a subluxation or dislocation episode.
Mechanism of Injury/Description: A patella subluxation or dislocation occurs when the patella (knee cap) comes out of the patellofemoral groove. Subluxation refers to the knee cap partially moving out of place while a dislocation means it has completely moved out of place. This can occur from a direct hit to the patella (knee cap) or from a noncontact extended (straight leg) plant and twisting motion.
Signs/Symptoms: Signs/symptoms of a patella subluxation or dislocation include experiencing acute/sudden pain, deformity, inflammation (swelling), feelings of instability or that the knee has “popped out.”
Diagnosis: The diagnosis of a patella subluxation or dislocation is determined by performing a physical exam which shows a positive apprehension test, inflammation (swelling) of the knee, tenderness to palpate on the MPFL, and a positive J sign. An x-ray will show a lateral patellar tilt (subluxation) or dislocation of patella (dislocation) from the patellofemoral groove. An MRI is also recommended to be ordered to evaluate for ligamentous, cartilage, loose bodies, and other injury to the knee.
Treatment: The treatment for a subluxation episode is rest from impact/pounding/landing, wearing a patellar stabilizing brace, and to work with physical therapy. For a dislocation, seek emergency treatment to have your knee (patella) put back into place and then once relocated a brace, and physical therapy are the main treatments but sometimes surgical intervention may be needed to stabilize your patella.
Prevention: To prevent this injury focus on VMO strength, stretching hip flexors and ITB, practice proper landing mechanics, and avoid valgus/knocked knees when landing.
Gymnastics Medical Provider PEARLS: If you are a medical provider the technique to relocate a dislocated patella is to straighten the knee and then use a knee immobilizer and transport to the local hospital/emergency department. Never perform any medical tests/treatments unless you are legally allowed to.
Gymnast, Parent, and Coach PEARLS: Gymnasts who continue to have subluxation episodes and have failed conservative treatment (rest, bracing, and PT) may require surgical stabilization. Talk with a pediatric sports medicine surgeon who reviews your options.
8
Patellar Subluxation/Dislocation
Patellar Subluxation/
Dislocation
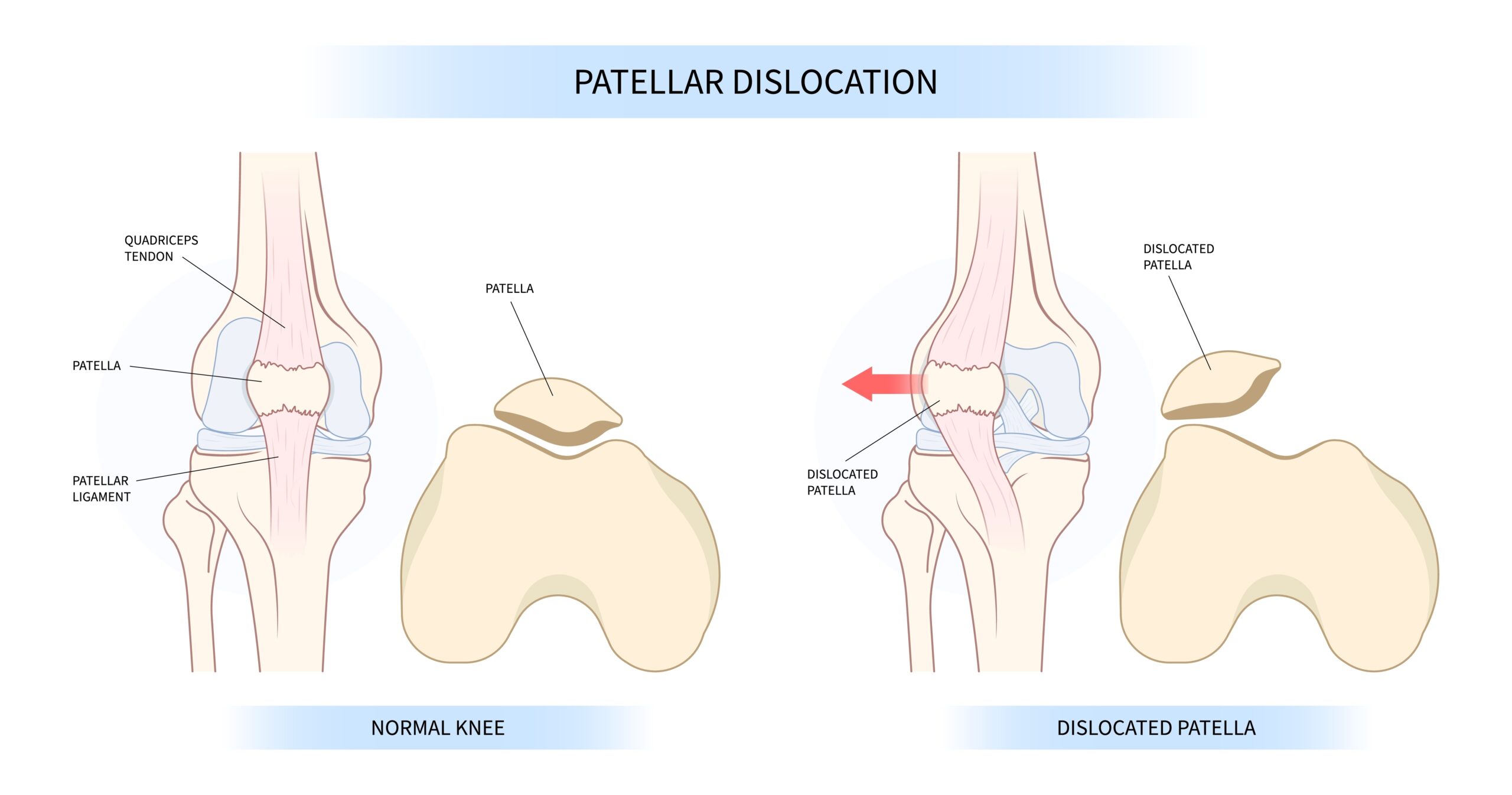
Epidemiology: A patella subluxation of dislocation can occur at any age. Some athletes may have “miserable malalignment syndrome” (external tibial torsion / pronated feet, genu valgum, and femoral anteversion) which predisposes them to having a subluxation or dislocation episode. Athletes who have patella alta (high riding patella), decreased VMO muscle bulk, and tight lateral structures are also predisposed to have a subluxation or dislocation episode.
Mechanism of Injury/Description: A patella subluxation or dislocation occurs when the patella (knee cap) comes out of the patellofemoral groove. Subluxation refers to the knee cap partially moving out of place while a dislocation means it has completely moved out of place. This can occur from a direct hit to the patella (knee cap) or from a noncontact extended (straight leg) plant and twisting motion.
Signs/Symptoms: Signs/symptoms of a patella subluxation or dislocation include experiencing acute/sudden pain, deformity, inflammation (swelling), feelings of instability or that the knee has “popped out.”
Diagnosis: The diagnosis of a patella subluxation or dislocation is determined by performing a physical exam which shows a positive apprehension test, inflammation (swelling) of the knee, tenderness to palpate on the MPFL, and a positive J sign. An x-ray will show a lateral patellar tilt (subluxation) or dislocation of patella (dislocation) from the patellofemoral groove. An MRI is also recommended to be ordered to evaluate for ligamentous, cartilage, loose bodies, and other injury to the knee.
Treatment: The treatment for a subluxation episode is rest from impact/pounding/landing, wearing a patellar stabilizing brace, and to work with physical therapy. For a dislocation, seek emergency treatment to have your knee (patella) put back into place and then once relocated a brace, and physical therapy are the main treatments but sometimes surgical intervention may be needed to stabilize your patella.
Prevention: To prevent this injury focus on VMO strength, stretching hip flexors and ITB, practice proper landing mechanics, and avoid valgus/knocked knees when landing.
Gymnastics Medical Provider PEARLS: If you are a medical provider the technique to relocate a dislocated patella is to straighten the knee and then use a knee immobilizer and transport to the local hospital/emergency department. Never perform any medical tests/treatments unless you are legally allowed to.
Gymnast, Parent, and Coach PEARLS: Gymnasts who continue to have subluxation episodes and have failed conservative treatment (rest, bracing, and PT) may require surgical stabilization. Talk with a pediatric sports medicine surgeon who reviews your options.
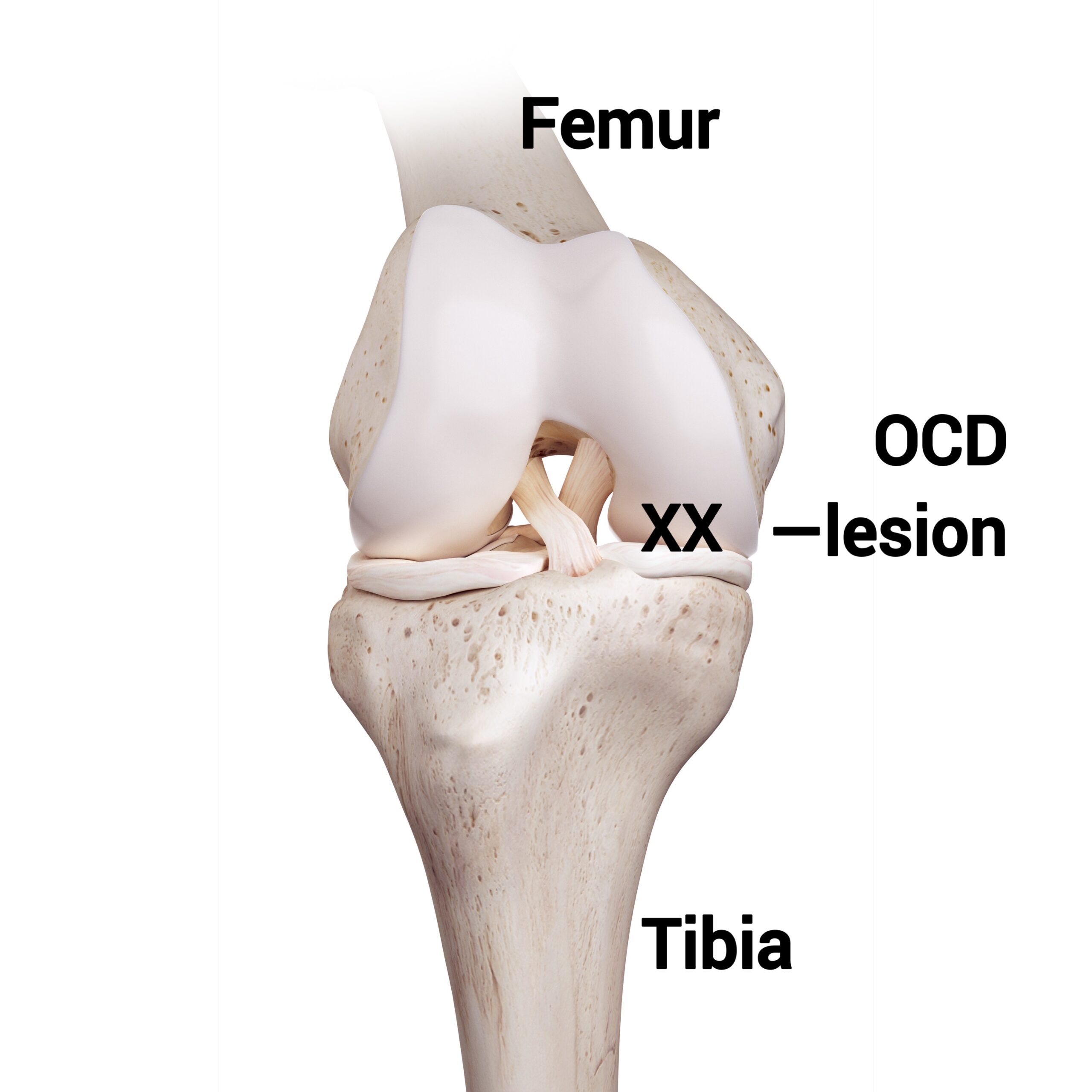
9
Osteochondritis Dissecans
ODC of the Knee
Epidemiology: OCD occurs in gymnasts with open growth plates, meaning they are still growing and have not yet finished going through puberty. The knee is the most common site for OCD specifically the medial femoral condyle followed by the lateral femoral condyle and lastly the trochlea.
Mechanism of Injury/Description: “A pathologic lesion affecting articular cartilage and subchondral bone” (OrthoBullets©). It is believed that OCD occurs from repetitive pounding and impacting on skeletally immature bones. It is also thought to be caused by trauma, hereditary, or vascular.
Signs/Symptoms: A gymnast with OCD of the knee will experience pain in the knee, usually described as a “deep ache”, have loss of motion (flexion or extension), have inflammation (swelling), and feel like the knee is “stuck” (mechanical signs/symptoms).
Diagnosis: The diagnosis of OCD is determined by performing a physical exam which shows the gymnast is missing flexion or extension, has swelling/inflammation, pain to palpation (touch), and a positive Wilson test. An x-ray, specifically a tunnel view, will show a “shark bite” or loose body on the medial femoral condyle, lateral femoral condyle, or trochlea. An MRI is then ordered and used to stage the lesion and help determine what treatment would be indicated.
Treatment: Treatment of OCD of the knee depends on the stage and location of the lesion. An earlier stage lesion that does not have a loose body can sometimes be treated with rest, crutches, and avoiding weight bearing/impact/pounding. In more severe cases (an unstable lesion), surgery is required.
Prevention: To prevent OCD lesions consider decreasing repetitive impact/pounding on growing bodies, allow time to rest between practices, rotating events/skills per practice/week, and practice proper landing mechanics.
Gymnastics Medical Provider PEARLS: Always start with x-rays (specifically tunnel/notch view) and if you do think you see an OCD lesion order an MRI to determine the stage of the lesion as this will help you determine the treatment.
Gymnast, Parent, and Coach PEARLS: In terms of prognosis the younger the athlete the better the prognosis. If the lesion in the lateral femoral condyle or trochlea these tend to have a worse outcome/poorer prognosis. Be sure your medical provider orders an MRI to stage your lesion and help determine your gymnast’s treatment plan.
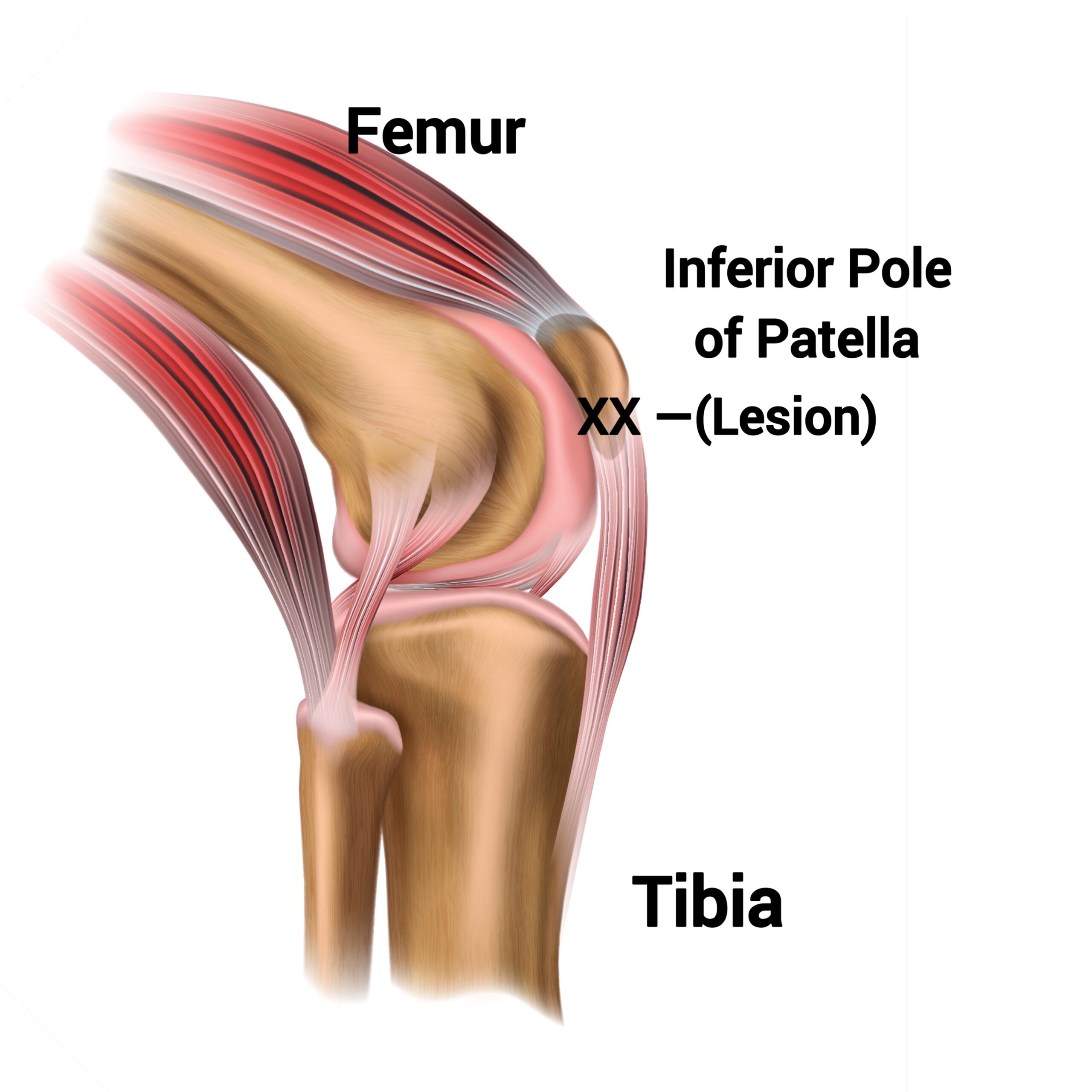
10
Inferior Pole of the Patella Apophysitis
Sinding Larsen Johansson
Epidemiology: This injury occurs in gymnasts with open growth plates, meaning they are still growing and have not yet finished going through puberty.
Mechanism of Injury/Description: An injury to the inferior pole of the patella from the patellar tendon “tugging”/contracting and pulling on the inferior pole of the patella (where there is a growth plate) causing inflammation and pain.
Signs/Symptoms: The gymnast will have anterior knee pain with tenderness to palpation (touch) on the lower portion of the knee cap (patella/inferior pole of the patella).
Diagnosis: The diagnosis is determined by physical exam (tenderness to palpate/push on the inferior pole of the patella, pain with resisted knee extension, and tight/inflexible quadriceps muscles/a positive Ely test), and a lateral x-ray may show widening at the inferior pole of the patella and this is important to view /obtain as there is a risk of a potential avulsion fracture if not treated.
Treatment: Treatment for Sinding Larsen Johansson is rest from pounding/impacting/landing, physical therapy (with a focus on quad/hip flexor flexibility, gluteus/hip strengthening, with proper landing mechanics), and then a gradual progression back to gymnastics.
Prevention: To prevent this injury focus on quadriceps flexibility and splits with square hips, decreasing repetitive impact/pounding on growing bodies, and practicing proper landing mechanics.
Gymnastics Medical Provider PEARLS: This injury tends to occur more in adolescents. Continue to monitor this injury as some gymnasts may try to ignore the pain and cause an avulsion fracture.
Gymnast, Parent, and Coach PEARLS: Gymnasts can try chopat© straps with either pre-wrap of the traditional strap to take “tension” off the tendon. Coaches, focus on your gymnasts having square hips when performing splits.